Principal Investigator: Matthew Maltese, PhD, Children’s Hospital of Philadelphia
Motor vehicle crashes are the leading cause of death for all children, and traumatic brain and skull injuries are the most common serious injuries sustained by children in motor vehicle crashes, both as vehicle occupants and pedestrians. The long term goal of this research is to elucidate the biomechanics of pediatric traumatic brain injury, and improve capability and accuracy of the ATD, injury assessment, and computer modeling tools available to the automotive safety research and engineering community.
Below is an executive summary of this line of research. Please note that each summary describes results and interpretation that may not be final. Final interpretation of results will be in the peer-reviewed literature.
Finite element (FE) modeling is a design tool that allows vehicle manufacturers to digitally develop safety systems and vehicle structures and to simulate crashes in the computer environment without the constraints of engineering materials, associated costs, and production time. This line of research aims to improve the FE model design tools available to engineers as they develop motor vehicle safety systems that mitigate traumatic brain injuries (TBI) in children. TBI, the most common serious injury sustained by children in motor vehicle crashes, can lead to neuropsychological effects, including altered behavior, diminished academic achievement, and increased family strain. Hospitalization costs associated with pediatric TBI are estimated to exceed $1 billion annually.
Specifically, researchers aimed to develop an FE model of the pre-adolescent human brain and skull and to demonstrate its usefulness in predicting brain deformation during real-world crash reconstructions.
2015-2016
Traumatic brain injuries (TBI) are the most common serious injuries sustained by children in motor vehicle crashes (MVCs), both as vehicle occupants and as pedestrians. Brain injuries are commonly associated with evidence of head contact with the vehicle interior, intruding door, or other exogenous sources in MVCs. To protect the brain, the Head Injury Criterion (HIC) was developed principally from direct head contact impact experiments with cadaver skulls. Child restraint system (CRS) performance standards and due care testing are implemented via a frontal impact sled test, anthropomorphic test devices (ATDs), also known as crash test dummies, and the HIC. But, because no head contact to exogenous structures occurs in these sled tests, the validity of the HIC is questionable. This research aimed to determine the relationship between HIC score and brain injury in head acceleration events with and without direct contact to the head.
Unlike skull fracture or other orthopedic injuries, understanding the complex relationship between impact biomechanics, physiology, and resulting brain injury requires a living organism (i.e., an animal model of TBI). Recently, University of Pennsylvania researchers have developed and refined an anesthetized porcine model of pre-adolescent TBI. This model reproduces the constellation of lesions and physiology that constitute human moderate-to-severe TBI and plays an essential role in validating the use of a finite element model (FEM) of the brain to predict brain injury.
In this study, investigators developed FEMs of the human brain at 1 year, 3 years, and 6 years to investigate brain injury potential in head acceleration events with and without head impact. Sled tests were conducted with and without head contact that produce similar HICs, and investigators compared brain tissue strain and strain rate for contact and non-contact events. Sled test results showed that the FE brain-estimated brain injury potential is greater when head contact occurs. More specifically, brain tissue maximum principal strain increased from 8 percent to 42 percent, and maximum principal strain rate increased from 242 percent to 582 percent in head contact cases compared with HIC- matched non-head contact cases.
This project delivers robust and useful 1-year-old, 3-year-old, and 6-year-old FE brain and skull models to the research and engineering community, and highlights important differences in injury potential in contact and non-contact head impact scenarios.
2014-2015
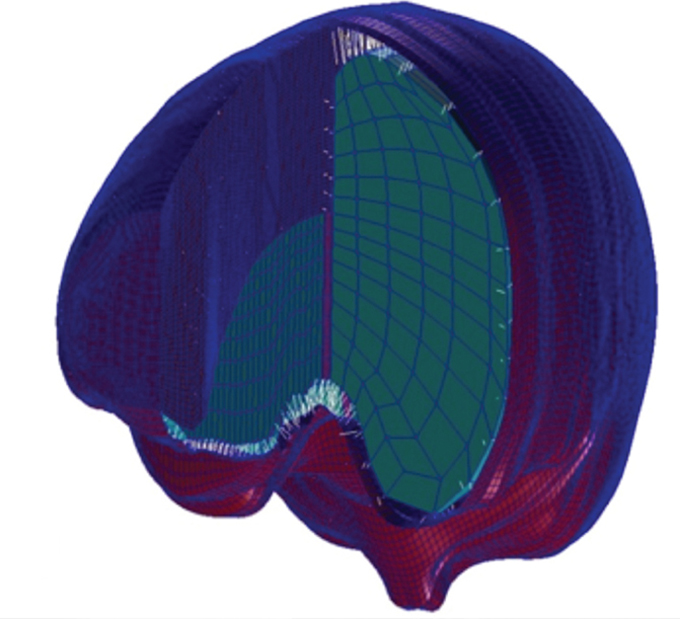
Right image: Right half of the finite element model showing distinct regions of white matter.
In Year 2, researchers added distinct regions of gray and white matter. Recent analyses of previously published animal data showed enhanced axonal injury prediction when only the white matter is examined. This brain model was then integrated with a skull model of the 6-year-old human based on published geometric and material data and was tested for predicting brain deformation during rapid rotation reconstructions. In these reconstructions, the FE brain model was rotated in each of the three anatomical planes: sagittal, axial, and coronal. Results showed that the axial and sagittal rotation directions had the highest strains.
This project delivers a pre-adolescent FE brain and skull model to the research and engineering community. This model may be used by other researchers to design and evaluate safety systems for the pre-adolescent age range, including assessing brain injury potential in pedestrian crash tests or designing side curtain air bags for children. This research lays a foundation to elucidate the biomechanics of pediatric TBI and to improve the capability and accuracy of the computer modeling tools available to the automotive safety research and engineering community.
2013-2014
In Year 1 of this project, researchers developed an FE model of the 6-year-old human brain that used an MRI averaging process to combine 26 individual segmented MRI brain scans. A pediatric 6-year-old human brain and skull FE model was developed based upon an average MRI scan template from the McConnell Brain Imaging Center of the Montreal Neurological Institute at McGill University. The usefulness of the model was then demonstrated in predicting brain deformation during rapid rotation reconstructions. The FE brain model was rotated in each of the three anatomical planes (sagittal rotations, axial rotations, and coronal rotations); results showed that the axial rotation direction had the highest strains. As part of a previous project funded by the National Highway Traffic Safety Administration (NHTSA), six real-world crashes were reconstructed with seat belt restrained rear-row pediatric occupants in the age and size range of the 6-year-old occupant in order to yield a range of likely head angular and linear acceleration time histories from each case. In the current project, these head acceleration time histories were used as the input to the FE brain model in order to translate global head kinematics to brain mechanics.
Four separate car crash reconstructions were chosen that represented a variety of crash conditions (frontal and side impact), with a range of occupant ages (6 to 10 years), and mild to moderate brain injury (Abbreviated Injury Scale maximum score of 2 to 5). Results showed that the two reconstructions with diffuse axonal injury had the highest strain. The next phase of this research will involve further development of the 6-year-old FE brain model by adding a deformable skull, and then using this new brain model to answer key questions in pediatric head injury mitigation that are most relevant to pediatric pedestrian and booster-seated occupant safety.
Project Team Members
Kristy Arbogast, PhD, Children’s Hospital of Philadelphia (Y1,Y2,Y3); Susan Margulies, PhD, The University of Pennsylvania (Y1,Y2,Y3); Iztok Ciglaric, PhD, Graz University of Technology (Y1).
Students
Christopher Polster, BS, Children’s Hospital of Philadelphia (Y1,Y2,Y3); Sriram Moparthy, BS, Children's Hospital of Philadelphia (Y2).
IAB Mentors
Mark Neal, General Motors Holdings LLC (Y1,Y2,Y3); Ann Mallory, Transportation Research Center Inc. (Y1,Y2,Y3); Uwe Meissner, Technical Advisor (Y1,Y2,Y3); John Combest, Nissan Technical Center North America Inc. (Y2, Y3); Hiromasa Tanji, TK Holdings Inc. (Y2,Y3); Eric Dahle, Evenflo Company Inc. (Y2,Y3); Guy Nusholtz, FCA US LLC (Y2,Y3); Steve Rouhana, Ford Motor Company (Y2).