Principal Investigator: Ashley Weaver, PhD, Wake Forest University
Below is an executive summary of this line of research. Please note that each summary describes results and interpretation that may not be final. Final interpretation of results will be in the peer-reviewed literature.
Because children are not simply “small adults,” the management of their unique injuries at trauma centers (TCs) must be approached differently. One of the most important factors in the treatment of traumatic injuries is the process of trauma triage, which involves transporting the “right patient” to the “right place” at the “right time.” However, trauma triage algorithms remain varied and stand to improve with the use of Advanced Automatic Crash Notification (AACN), which utilizes information retrieved by a vehicle’s Event Data Recorder to predict the severity of injuries sustained by occupants and subsequently alert first responders to the event in real time. Though several research groups have developed AACN algorithms for adults, none have yet been developed for children. Given children’s constant growth and development, there is a need for a pediatric-specific AACN system that can adjust its injury risk prediction based upon their developmental stage.
The long-term goal of this project is to create a pediatric-specific AACN algorithm that uses a more comprehensive scoring system than the Abbreviated Injury Scale (AIS) to predict the risk that a child in a motor vehicle crash (MVC) is severely injured and requires treatment at a designated TC.
2016-2017
CONTEXT
Motor vehicle crashes (MVCs) remain a leading cause of death and disability in children worldwide. Prompt field triage of seriously injured children to designated trauma centers (TCs) improves outcomes. Advanced Automatic Crash Notification (AACN) systems improve the speed and accuracy of field triage decisions. Previous AACN algorithms have been created for adults and have used Abbreviated Injury Scale (AIS)-based severity metrics to define severely injured patients requiring treatment at designated TCs. Use of such algorithms in children is problematic for two main reasons. First, children are constantly growing and developing and this affects the injuries incurred. Thus, creation of a pediatric AACN algorithm will require data-driven quantification of the risks of particular injury types in MVC occupants across changing developmental metrics. Second, the AIS severity grading system was originally created for use in adults and offers no mechanism for accounting for the developmental stage of the child. Developmental stage may affect the physiologic responses and resultant severity of injury.
PROJECT OBJECTIVES
The long-term goal of this project is to create a pediatric-specific AACN algorithm that uses a more comprehensive scoring system than AIS to predict the risk that a child in a MVC is severely injured and requires treatment at a designated TC.
METHODS
A list of injuries associated with a pediatric patient’s need for Level I/II TC treatment known as the Target Injury List was determined using an approach based on 3 facets of injury: severity, time sensitivity, and predictability. The inputs used to create the pediatric-specific AACN algorithm include the Target Injury List and 12,058 MVC occupants from the National Automotive Sampling System-Crashworthiness Data System (NASS-CDS) 2000-2014. The algorithm uses multivariable logistic regression to predict an occupant's risk of sustaining an injury on the TIL from the following input variables: delta-v, number of quarter turns, belt status, multiple impacts, airbag deployment, and age group. Two separate versions of the algorithm were developed: one with belt status as a model parameter and one with no belt status included. The pediatric-specific AACN was optimized in order to minimize under triage (UT) and over triage (OT) rates with the goal of producing UT rates < 5% and OT rates < 50% as recommended by the American College of Surgeons (ACS).
RESULTS
For the algorithm with belt status included as a model parameter, the OT rates were 44% (frontal), 47% (near side), 43% (far side), 25% (rear), and 49% (rollover). The UT rates for this algorithm were 3% (frontal), 3% (near side), 2% (far side), 8% (rear), and 14% (rollover). For the algorithm with belt status not included as a model parameter, the OT rates were 49% (frontal), 49% (near side), 38% (far side), 40% (rear), and 49% (rollover). The UT rates for this algorithm were 5% (frontal), 6% (near side), 5% (far side), 23% (rear), and 32% (rollover). Note there are not separate algorithms for each of the developmental age groups (due to sample size limitations), but these results are for the pediatric population as a whole.
CONCLUSIONS
Injury patterns change as children grow and develop. Current AACN algorithms in industry are not pediatric specific. The developed pediatric-specific AACN algorithm uses measurements obtainable from vehicle telemetry to predict risk of overall occupant injury and recommend a transportation decision for the occupant. The AACN algorithm developed in this study will aid emergency personnel in making the correct triage decision for an occupant after a MVC, and once incorporated into the trauma triage network it can reduce response times, increase triage efficiency, and improve overall patient outcome.
2015-2016
where MP = predictability score multiplier; Ms = severity score multiplier; MTS = time sensitivity score multiplier;
NASS-CDS = National Automotive Sampling System - Crashworthiness Data System; NIS = Nationwide Inpatient Sample;
NTDB = National Trauma Data Bank; and TC = trauma center.
Motor vehicle crashes (MVCs) remain a leading cause of death and disability in children worldwide. Prompt field triage of seriously injured children to designated trauma centers (TCs) can improve outcomes, and these decisions can be streamlined with the use of Advanced Automatic Crash Notification (AACN) systems to improve speed and accuracy.
The long-term goal of this project is to create a pediatric-specific AACN algorithm that uses a more comprehensive scoring system than the Abbreviated Injury Scale to predict the risk that a child in a MVC is severely injured and requires treatment at a designated TC. Year 1 of this project evaluated the most common injuries occurring in children and delineated the specific ways in which the incidence of these injuries change as children grow and develop, while Year 2 focused on refining the injury patterns to create a better understanding of the pediatric injuries described in the first phase.
In Year 3, a list of injuries associated with a pediatric patient’s need for Level I/II TC treatment known as the Target Injury List was determined using an approach based on three facets of injury: severity, time sensitivity, and predictability. The inputs used to create the pediatric-specific AACN algorithm include the Target Injury List and 11,632 MVC occupants from the National Automotive Sampling System-Crashworthiness Data System 2000-2011. The algorithm uses multivariable logistic regression to predict an occupant's risk of sustaining an injury on the Target Injury List from various crash-related input variables. Two separate versions of the algorithm were developed: one with belt status as a model parameter and one with no belt status included. The pediatric-specific AACN was optimized in order to minimize under triage (UT) and over triage (OT) rates with the goal of producing UT rates < 5 percent and OT rates < 50 percent, as recommended by the American College of Surgeons.
For the algorithm with belt status included as a model parameter, the OT rates were <50 percent for all crash modes. The UT rates for this algorithm were <5 percent for frontal, near, and far side crashes. For the algorithm with belt status not included as a model parameter, the OT rates were <50 percent for all crash modes The UT rates for this algorithm were <5 percent for near and far side crashes.
The AACN algorithm developed in this study will aid emergency personnel in making the correct triage decision for an occupant after a MVC and, once incorporated into the trauma triage network, can reduce response times, increase triage efficiency, and improve overall patient outcomes.
2014-2015
Year 2 of the project focused on refining the injury patterns to create a better understanding of the pediatric injuries described in the first phase. Researchers performed a retrospective review of injuries to occupants 19 years old and under in crashes contained within the 2000-2011 National Automotive Sampling System – Crashworthiness Data System (NASS-CDS) dataset. Results from logistic regression models predicting 18 key injury types were compared to determine which metrics should be used as co-variates in a pediatric AACN algorithm. Injury patterns were then used to create developmental groupings that discriminated between pattern categories. Researchers conducted advanced data mining and statistical analysis of several large national databases and survey data to define the severity, time sensitivity, and predictability of the most frequently occurring MVC-induced injuries within each developmental group, which were then combined to create age specific Target Injury Scores (TIS) for the most common MVC-induced pediatric injuries.
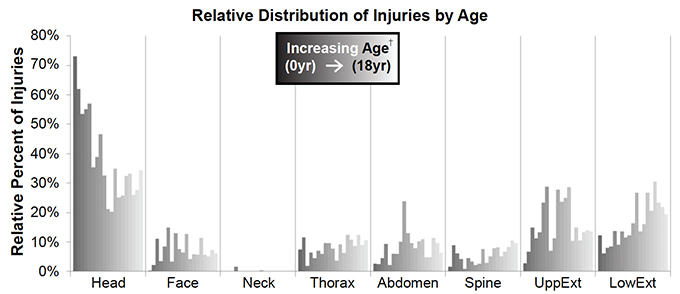
The results from this current study reveal that age alone provides the best predictive power with respect to injury patterns. Researchers established four pediatric age groups using injury patterns to differentiate between injury types (0-4; 5-9; 10-14; 15-18). Analyses showed that younger children were at increased odds of sustaining Abbreviated Injury Scale (AIS) 2+ and 3+ head injuries and AIS 3+ spinal injuries. Older children were at increased odds of sustaining chest wall fractures, AIS 3+ abdominal injuries, and AIS 2+ upper and lower extremity injuries. Overall, TIS values decreased with increasing age, and increasing AIS severity correlated with increasing TIS within each age group.
Injury patterns change as children grow and develop, and age proved to have the best predictive power. Triage may be improved with the use of age-adjusted TIS values to help discriminate between those children who require TC care and those who can be safely managed at a non-TC. Year 3 will utilize these scores to create age-specific AACN algorithms.
2013-2014
by age in the NASS-CDS 2000-2011 dataset.
Year 1 of this project evaluated the most common injuries occurring in children and characterized them across different developmental groups. Specifically, this project focused on quantification of the patterns of injuries among pediatric MVC occupants as they grow in age, height and weight; and preliminary assessment of the severity, time sensitivity and predictability of the most common injuries sustained among MVC occupants in different pediatric age groups.
The research team conducted a retrospective review of occupants 0-18 years of age with injuries of AIS 2+ severity using the National Automotive Sampling System – Crashworthiness Data System (NASS-CDS) 2000-2011 dataset to determine the most common MVC- induced injuries occurring in each developmental group. The results of the analysis showed that injury patterns change as children grow and develop. In general, the odds of head injury significantly decreased during development, while the odds of spinal injury, thoracic wall fracture and lower extremity fracture increased during development. Given the uniqueness of the different stages of pediatric development, age groupings (0-4, 5-9, 10-14 and 15-18 years) were established to allow for the creation of more specific algorithms within each developmental group. Having a system that links an age group with relative risk of various injury types will have important implications for clinicians, improving time, cost-effectiveness and, most importantly, pediatric patient care.
Project Team Members
Ryan Barnard, MS, Wake Forest University (Y1, Y2, Y3, Y4); Jennifer Talton, MS, Wake Forest University (Y1, Y2, Y3, Y4)
Students
Samantha Schoell, Wake Forest University (Y1, Y2, Y3, Y4); Daniel Cheng, Wake Forest University (Y1)
IAB Mentors
Doug Longhitano, American Honda Motor Co., Inc. (Y3, Y4); Eric Dahle, Evenflo Company Inc. (Y3, Y4); John Combest, Nissan Technical Center North America Inc. (Y3, Y4); Hiromasa Tanji, TK Holdings Inc. (Y3, Y4); Dan Robertson, Toyota USA (Y1, Y2, Y3, Y4); Uwe Meissner, Technical Advisor (Y1, Y2, Y3, Y4); Jerry Wang, Humanetics Innovative Solutions Inc. (Y1); Julie Kleinert, General Motors Holdings LLC (Y1); Christina Mullen, State Farm Mutual Automobile Insurance Company (Y1, Y2); Michelle Caldwell, Childress Institute for Pediatric Trauma (Y1); Agnes Kim, Ford Motor Company (Y2); Steve Rouhana, Ford Motor Company (Y1).
Publication References